DistressRx™ for Employee Health, Vitality, & Burnout Prevention for Organizations.
12-Week Education & Coaching Curriculum led by The Fit Collective®.
Our program teaches doctors how to turn emotional stress into leadership power. Instead of just trying to "push through" hard feelings like frustration or burnout, you'll learn how to understand these feelings and use them to grow. We call this DistressRx™.
DistressRx™: Turning Emotional Stress into Leadership Power
Why This Work Matters
Physician attrition is one of the most urgent and costly challenges facing healthcare organizations today. The loss of a single physician—often estimated between $500,000 and over $1 million—extends far beyond recruitment expenses. It disrupts continuity of care, erodes team morale, and weakens organizational culture.
At the core of attrition are burnout, moral distress, and chronic emotional exhaustion. Yet many institutional responses focus on surface-level interventions—wellness seminars, resilience talks, or temporary time off—without addressing the underlying emotional drivers that cause physicians to disengage in the first place.
Our Solution: DistressRx™
DistressRx™ is a next-generation approach to physician well-being, leadership development, and retention. Rather than teaching physicians to suppress or “push through” stress, DistressRx™ equips them to transform emotional distress into clarity, agency, and leadership capacity.
Through DistressRx™, physicians learn how to:
Understand the purpose and signaling role of difficult emotions
Identify their personal Transform Tolerance™ subtype
Regulate emotional distress with practical, evidence-informed tools
Translate internal conflict into professional clarity and decisiveness
Expand leadership capacity by resolving inner resistance
This work does not aim to eliminate stress. Instead, it reframes stress as actionable data—an opportunity for growth, alignment, and leadership development.
Impact on Engagement and Retention
When physicians are taught how to process and repurpose emotional stress, the effects extend well beyond individual well-being. Participants consistently experience:
Reduced burnout and emotional exhaustion
Greater sense of control, agency, and confidence
Improved communication and conflict navigation
Stronger alignment with organizational values
Renewed engagement and meaning in their work
These outcomes translate into higher job satisfaction, stronger institutional loyalty, and improved long-term retention.
A Strategic Fit for Health Systems
DistressRx™ aligns naturally with core organizational priorities, including:
Clinician well-being and sustainability
Leadership development and succession planning
Psychological safety and team culture
Diversity, equity, and inclusion (DEI) initiatives
Cost containment through reduced attrition
By reframing emotional stress as a leadership asset rather than a liability, DistressRx™ helps organizations move beyond burnout mitigation toward true professional thriving.
Investing in DistressRx™ is not simply an investment in retention—it is an investment in a resilient, self-aware, and empowered physician workforce built from the inside out.
DistressRx™ with Transform Tolerance™
A Proven Retention Strategy for Physicians
Where the Distress Types Come From
The seven Transform Tolerance™ Distress Types were identified through years of coaching and working alongside thousands of high-achieving women physicians. These patterns emerged consistently across clinical decision-making, leadership roles, team dynamics, and moments of profound professional stress.
Rather than viewing emotional reactions as lapses in professionalism or personal weakness, the Transform Tolerance™ framework recognizes distress responses as adaptive survival strategies developed in high-stakes, high-accountability environments. What once protected physicians under pressure can later become a source of burnout, disconnection, and disengagement if left unexamined.
DistressRx™ helps physicians identify the underlying intolerance driving their distress—such as fear of being wrong, exposed, unsupported, or out of control—and retrain these patterns into regulated, leadership-aligned responses. This shift supports sustainable performance, stronger professional identity, and long-term commitment to one’s role.
The Retention Practice Gap
Women physicians often practice in emotionally intense environments with limited support for managing internal stress responses. Over time, this leads to:
Escalating burnout and emotional exhaustion
Disconnection from team, mission, and leadership identity
Quiet quitting, role disengagement, or active job seeking
Without tools to process distress in real time, physicians either exit the profession or remain physically present while emotionally withdrawn.
DistressRx™ with Transform Tolerance™ directly addresses this retention gap by giving physicians practical, repeatable tools to reframe emotional stress as a signal for growth—extending both career longevity and leadership capacity.
Learning Objectives (Retention-Centered)
By the end of the DistressRx™ program, physicians will be able to:
Identify their unique Transform Tolerance™ Distress Type and its impact on work-related stress
Reframe emotional reactions as leadership data rather than threats
Apply emotional regulation strategies during clinical, interpersonal, and leadership stress
Strengthen boundaries and improve team communication
Restore meaning, agency, and purpose in their current roles
Reduce emotional exhaustion, supporting engagement and retention
Program Features That Support Retention
Targeted coaching tailored to each distress subtype
Self-assessment quiz with personalized insight report
Practical tools to pause, reframe, and respond under pressure
Strategies addressing numbness, anger, perfectionism, and isolation
Designed specifically for women physicians in high-pressure clinical and leadership roles
Distress Patterns That Predict Attrition
Transform Tolerance™ identifies specific distress patterns that, when unaddressed, strongly correlate with burnout, disengagement, and intent to leave. DistressRx™ intervenes early—before emotional strain becomes institutional loss.
Outcome Measures with Retention Focus
1. Self-Awareness Growth (Leading Indicator of Retention)
Increased recognition of stress patterns
Greater insight into internal drivers of burnout
Goal: +1.5-point increase in emotional self-awareness scores
2. Behavioral Change
Consistent use of stress-to-leadership tools
Improved boundaries and coping behaviors
Goal: 70–80% active behavioral adoption
3. Clinical and Team Impact
Greater presence during patient care
Fewer stress-driven interpersonal conflicts
Goal: +1.5-point improvement in leadership and collaboration metrics
4. Burnout Reduction
Reduced emotional exhaustion and depersonalization
Renewed connection to purpose in medicine
Goals:20% reduction in burnout symptoms
85% report increased job satisfaction
5. Retention & Institutional ROI
Improved physician retention at 6–12 months
Decreased intent to leave organization or profession
Program Outcomes
Most physicians stay: 8–9 out of every 10 participants remain in their roles
Significant organizational savings: $5–10 million preserved for every 10 physicians retained
High completion rates: Over 90% of physicians successfully complete the program
DistressRx™ Program: Early Pilot ROI Outcomes from 100 Physicians
Strong Results. Real Retention. Proven ROI.
Preliminary data from 100 physicians who completed the Transform® coaching program show powerful results across clinical skill, emotional resilience, and—most importantly—job retention.
Retention Outcomes: A Direct Investment Return
84% of doctors reported they are more likely to stay in their current job.
84% said they are less likely to leave medicine altogether.
These results reflect significant improvements in job satisfaction and emotional endurance—two of the biggest drivers of physician attrition.
Estimated ROI:
Replacing a single physician can cost up to $1 million.
If just 81 of the 100 participating physicians stay, this represents an organizational savings of $40–$81 million.
Statistically Validated Impact
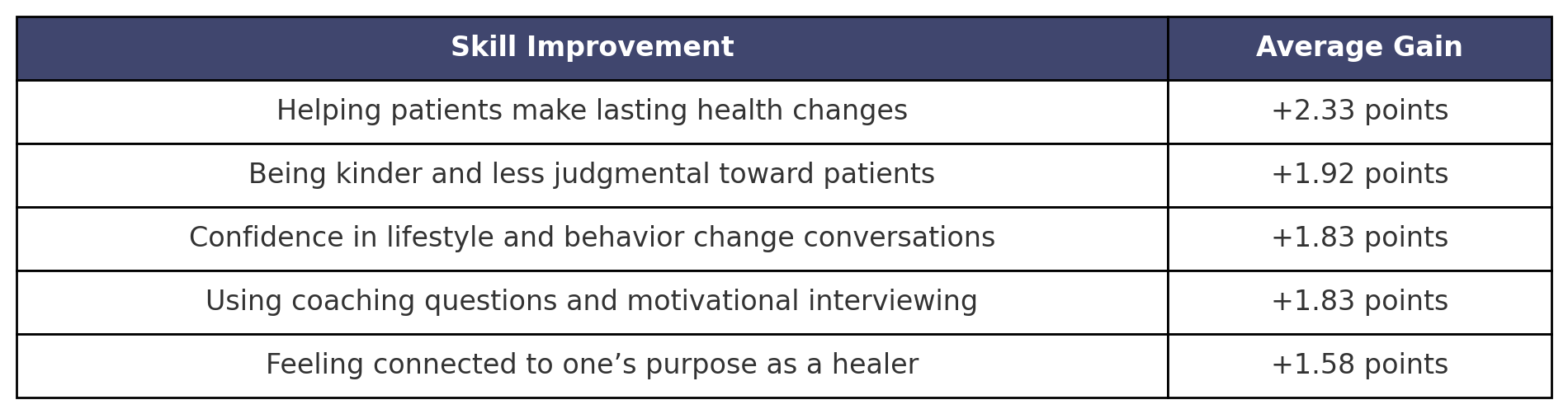
Doctors showed measurable improvement in every skill assessed—with average increases ranging from +1.4 to +2.3 points on a 5-point scale. These shifts reflect movement from “sometimes” to “often” or “almost always” experiencing confidence in their clinical and leadership roles.
The results were statistically robust, confirmed by t-statistics > 11 and p-values < 0.00000000001.
Key Skills That Drove Retention & Performance
These changes weren’t just “nice to have”—they helped physicians feel healthier, stronger, and more aligned with their purpose, leading directly to greater career longevity.
Participant Reflections
“I feel like a true model of health.”
“Transform® gave me the confidence to walk the talk—with full integrity.”
“I’m more present and patient—with myself and my patients.”
“My stress response is better. That shows up in my care.”
“Perfection isn’t required—just progress.”
“I help my patients embrace sustainable change. That starts with me.”
“My clinical conversations have completely changed.”
“Open-ended coaching questions have deepened patient trust.”
“I’ve found balance—and I’m sharing that with my patients.”
“This program improved my own health, which improves theirs.”
Bottom Line for Organizations
Among 97 physicians who completed the program:
81 physicians (84%) scored 4/5 or 5/5 on at least two of the three key retention indicators:
–After Transform®, more likely to remain in current job (4.13)
–After Transform® more likely to stay in the practice of medicine (4.19)
–After Transform® more Job satisfaction based on focusing on controllables (4.20)
–T > 11, p < 0.000000000000001
84% improved retention intention
$40M–$81M in estimated cost savings per 100 physicians
Clinically validated and statistically significant results
Built-in CME, lifestyle medicine, and emotional resilience tools
➡️ Transform® doesn’t just help doctors feel better—it helps systems keep their best people.
DistressRx™ Institutional Program Structure
A Comprehensive, Customizable Retention & Leadership Solution
Program Overview
DistressRx™ is a 12-week live institutional program designed to reduce burnout, strengthen leadership capacity, and improve physician retention—with year-long strength training program and replays plus cliff notes provided for each session.
The program integrates:
Emotional regulation and leadership development (DistressRx™)
Evidence-informed metabolic health nutrition strategy
Progressive, time-efficient strength training to support resilience and longevity
All components are fully customizable to align with your institution’s priorities, culture, and strategic goals.
Clinician Health & Vitality
The Distress Rx: A 12-Week Advanced Stress Curriculum for Clinicians
Week 1: Stress, the Clinician Body, and the Cost of Chronic Activation
Education
Stress physiology in clinicians: HPA axis, autonomic tone, cognitive load
Introducing The Stress Scale: acute vs chronic vs cumulative stress
Why high-functioning clinicians often miss early warning signs
Coaching Focus
Identifying your current stress baseline
Separating “busy” from biologically overloaded
Worksheet
Personal Stress Scale self-assessment
Early stress signals + current coping patterns
Live Q&A
Normalizing stress signals without pathologizing competence
Week 2: CBT & Thought Distortions in Clinical Stress
Education
Core CBT principles: thoughts, emotions, behaviors
Common clinician thought distortions (responsibility inflation, catastrophizing, perfectionism)
Why cognitive tools alone fail under physiological overload
Coaching Focus
Applying CBT to clinical stress, decision fatigue, and self-talk
Learning when thinking differently helps—and when it doesn’t
Worksheet
Thought–emotion–behavior mapping (clinical scenarios)
Distortion identification + reframe practice
Live Q&A
Reducing self-criticism without reducing standards
Week 3: DBT Skills for High-Stakes Clinical Environments
Education
Distress tolerance vs emotional regulation
DBT skills most relevant to clinicians (STOP, TIPP, Wise Mind, Self-Validation)
Why regulation must precede cognition under high stress
Coaching Focus
Selecting the right DBT skill for the moment
Staying regulated without disengaging or numbing
Worksheet
DBT skill decision tree for real clinical moments
Personal regulation toolkit
Live Q&A
Using DBT without feeling “therapeutic” or awkward
Week 4: The Stress Scale — Calibration, Drift & Recovery
Education
Deep dive into the Stress Scale
How clinicians drift from acute → chronic → cumulative stress
Why recovery fails when stress is misclassified
Coaching Focus
Accurately locating yourself on the Stress Scale
Matching interventions to stress level, not willpower
Worksheet
Stress Scale recalibration exercise
Mismatched coping audit (what you’re using vs what you need)
Live Q&A
Stopping inappropriate self-prescriptions
Week 5: Stress Types & How Clinicians Cope
Education
Overview of clinician stress response types
How stress shows up differently in leadership, caregiving, control, avoidance, urgency
Strengths that become liabilities under pressure
Coaching Focus
Identifying your dominant stress response
Recognizing blind spots without shame
Worksheet
Stress Type identification + reflection
Regulation strategies matched to type
Live Q&A
Letting go of “this is just how I am”
Week 6: The Relationship Stress Matrix — Part 1 (Awareness)
Education
How stress types interact relationally
Clinician–patient, clinician–team, clinician–self dynamics
Why misalignment creates friction, resentment, and exhaustion
Coaching Focus
Identifying recurring relational stress patterns
Understanding impact vs intent
Worksheet
Personal Relationship Stress Matrix
One relationship stress insight
Live Q&A
Seeing patterns instead of blaming people
Week 7: The Relationship Stress Matrix — Part 2 (Repair & Boundaries)
Education
Repair vs rupture in stressed relationships
Boundary failures as stress signals, not character flaws
Why some stress type pairings require structure, not conversation
Coaching Focus
Practicing stress-aware communication
Choosing the right repair strategy for the pairing
Worksheet
One relationship reset plan
Boundary reinforcement script by stress type
Live Q&A
Repairing without over-functioning
Week 8: Stress Sense — Part 1 (Interoception & Awareness)
Education
Stress sensing vs stress suppression
Interoception, body cues, and early warning signals
Why clinicians lose stress sensing capacity over time
Coaching Focus
Relearning how stress shows up before breakdown
Differentiating fatigue, overload, and shutdown
Worksheet
Stress signal inventory (body, emotion, behavior)
Early intervention mapping
Live Q&A
Trusting subtle signals again
Week 9: Stress Sense — Part 2 (Prediction & Prevention)
Education
Stress pattern recognition over time
Predictable stress cycles in clinical work
Why prevention is a skill, not a personality trait
Coaching Focus
Anticipating stress rather than reacting to it
Designing proactive regulation plans
Worksheet
Stress forecast exercise
Pre-stress regulation plan
Live Q&A
Staying ahead without hypervigilance
Week 10: Stress Tools — Matching Tool to Stress State
Education
Why most stress tools fail (wrong tool, wrong time)
Cognitive, physiological, relational, and structural tools
The danger of tool overload
Coaching Focus
Building a minimal, effective stress toolkit
Knowing when to stop adding and start subtracting
Worksheet
Tool-to-stress-state matching guide
Personal “do less, better” toolkit
Live Q&A
Simplifying without losing effectiveness
Week 11: Repairing Teams Through Stress Type Awareness
Education
How team dysfunction is often stress-type mismatch
Common clinical team stress collisions
Why personality labels fail but stress patterns help
Coaching Focus
Reducing conflict without forcing sameness
Leading repair conversations with clarity
Worksheet
Team Stress Type Map
One team repair strategy
Live Q&A
Leading without carrying everyone
Week 12: Building Teams Using Stress Type Intelligence
Education
Stress-aware team design
Role alignment, communication norms, and escalation paths
Sustainable leadership through regulation, not control
Coaching Focus
Designing teams that buffer stress rather than amplify it
Clarifying your leadership stress signature
Worksheet
Stress-intelligent team blueprint
One structural change to implement
Final Live Q&A + Reflection
Integration, identity shift, and forward application
IMPACT
By the end of this 12-week Distress Rx, clinicians no longer manage stress reactively.
They read it, predict it, communicate through it, and design systems around it—for themselves, their teams, and their patients.
Program Design Notes
Weekly live education with Q&A
Built-in coaching integration
Practical worksheets each week
Designed for clinician schedules
Supports personal health + better patient care
Monthly C-Suite–specific calls
12-Week Nutrition & Exercise Program
Onboarding & Intro Session
Group onboarding during the first live call
Establish baseline minimum commitment for exercise
Teach simple, effective nutrition strategy
Program Delivery
All workouts delivered asynchronously in The FIT Collective® App
Investment
Institutional Investment is custom quoted. Please submit form to so that we can contact you for further details.
Includes
12-week live DistressRx™ program
3 executive calls with the admin team/c-suite to target specific goals
Curriculum customization to institutional priorities
12-week strength training program
Continuation options
Pre- and post-surveys to assess program effectiveness
ROI Context
Retaining even one additional physician often offsets the entire program cost. Retaining multiple clinicians results in millions in avoided replacement expenses.
Why Institutions Choose DistressRx™
Addresses burnout at the root emotional level
Integrates mental, physical, and professional resilience
Scales efficiently across large organizations
Aligns with retention, leadership, DEI, and well-being priorities
Moves beyond wellness toward measurable institutional impact